From khaleejtimes.com
Psychiatrists and neurologists explain how prolonged sitting can worsen ADHD symptoms, trigger sciatica pain and reduce mental alertness
Doctors say this experience, often reported by people with ADHD or sciatica, has a clear biological explanation: when the body stops moving, the brain receives fewer signals to stay alert, gradually shifting into a low-energy, drowsy state. At the same time, sitting places mechanical stress on the spine and nerves, which can aggravate pain conditions such as sciatica.
While doctors have long warned against sitting for long periods, according to Dr Muhammad Farhan, Staff Physician at the Psychiatry & Behavioural Health Department of Cleveland Clinic Abu Dhabi’s Neurological Institute: “People need to move. The brain and the body are not designed to stay still for hours at a time.”
Why prolonged sitting worsens sciatica pain
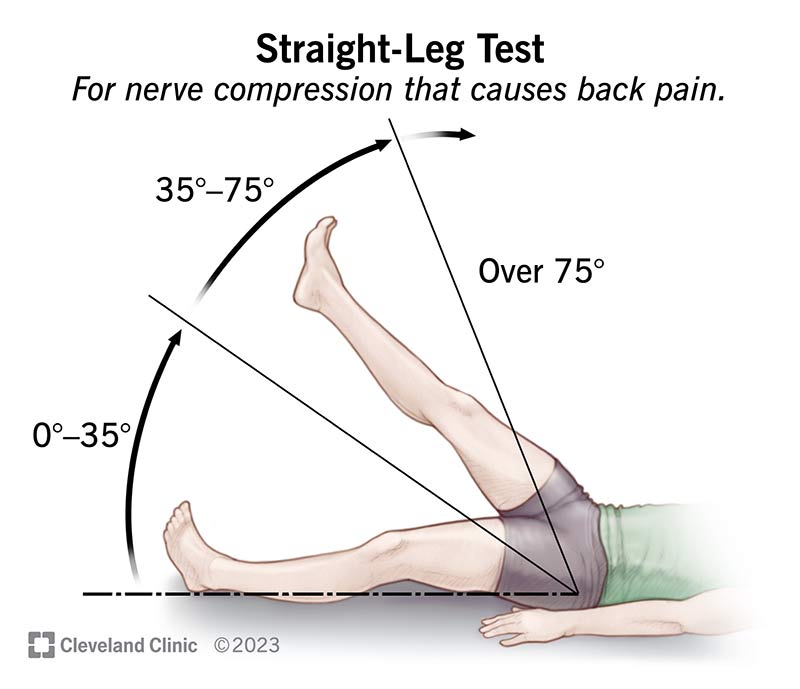
From a physical standpoint, prolonged sitting is particularly problematic for people with sciatica, a condition caused by irritation or compression of the sciatic nerve, which runs from the lower spine down the leg.
Dr Farhan explained that sitting for long periods can compress the sciatic nerve either at the level of the spine — especially in people with disc bulges — or as the nerve passes beneath muscles in the hip. “When you sit, the hips are flexed, and that position can increase pressure on the nerve,” he said. “That’s why pain, numbness or tingling in the leg often gets worse the longer someone sits.”
Neurosurgical specialists see this pattern frequently. According to Dr Nader Hebala, staff physician at Cleveland Clinic Abu Dhabi’s Neurological Institute, prolonged sitting increases pressure on the lower spine, especially when posture deteriorates over time.
“For people with sciatica or lower back pain, sitting places additional stress on the nerve roots that form the sciatic nerve,” Dr Hebala said. “Many patients notice that prolonged sitting worsens back or leg pain, particularly when posture is poor.”
This is why sit-stand desks and regular posture changes are often recommended. “Even a simple five-minute stand, walk or stretch can make a meaningful difference,” Dr Hebala added.
The brain’s ‘low-energy mode’
The impact of prolonged sitting goes beyond pain.
According to Dr Farhan, the brain relies on constant feedback from muscles and joints to maintain alertness. “When we sit still for long periods, there is less sensory input going to the parts of the brain that promote wakefulness,” he explained. “As a result, the brain shifts toward a lower-energy, drowsy state.”
This effect is linked to the brain’s natural sleep–wake rhythm, which is regulated not only by light but also by physical activity. “Movement during the daytime tells the brain that it is time to be awake and alert,” Dr Farhan said. “When activity drops, alertness drops.”
Brief movement — such as standing up, walking, or pacing — increases blood flow to the brain and stimulates the release of neurotransmitters such as dopamine and norepinephrine, both of which are essential for attention, motivation and wakefulness.
Why ADHD brains struggle with sitting
For people with ADHD, the problem is often amplified.
“In ADHD, the brain already has lower levels of dopamine and norepinephrine in areas responsible for focus and attention,” Dr Farhan explained. “Sitting still for long periods makes it even harder to maintain focus.”
Many patients with ADHD report that they think better when standing or walking — an observation supported by clinical experience. “For them, movement is not a distraction,” Dr Farhan said. “It is a form of self-regulation.”
Physical activity and posture changes increase dopamine and norepinephrine levels, improving motivation, mood and alertness. “That’s why people with ADHD often feel less restless, more focused and mentally clearer when they are on their feet,” he added.
Sitting, sleepiness and monotony
The same mechanisms help explain why prolonged sitting — especially during long drives — can lead to dangerous levels of sleepiness.
“Sitting combines immobility with monotony and reduced sensory input,” Dr Farhan said. “That combination lowers mental alertness.”
Coffee and stimulants may offer temporary relief, but they are not reliable solutions. “If someone feels sleepy, the safest option is to stop, take a break, get out of the car and move,” he said. “Movement tells the brain it is not time to sleep.”
Excessive daytime sleepiness may also point to underlying sleep disorders, which should be medically evaluated.
Balance, not extremes
While standing offers benefits, doctors stress that the goal is not to replace sitting entirely.
“Standing for long periods can also lead to fatigue if the body isn’t supported,” Dr Hebala said. “The key is balance — alternating between sitting and standing, maintaining good posture, and building regular movement breaks into the day.”
A practical guideline for most people is to change position every 30 to 45 minutes, combined with regular walking, stretching and exercise.
“The human brain is designed for movement,” Dr Farhan said. “Movement is not a break from thinking — it is how we stay awake, focused and neurologically healthy.”
Rethinking design
The discussion around prolonged sitting also raises broader questions about how everyday spaces are designed — from workplaces and conferences to long-distance travel.
For instance, when asked if cars that allow drivers to stand rather than sit could be a way to improve alertness during long journeys, Dr Farhan said: “That’s a very novel idea”, noting that prolonged seated driving combines immobility and monotony — a combination known to reduce alertness.
However, he stressed that any such concept would raise complex safety and policy considerations and would require extensive research before being considered viable.
What doctors were more confident about was the need for movement breaks. “If someone feels sleepy while driving, the only thing that truly works is stopping, getting out of the car and moving,” Dr Farhan said.
Another proposal was whether people with ADHD should be formally accommodated in environments where sitting is mandatory — such as conferences, lectures or even flights — particularly when no standing options are available. Dr Farhan said that, clinically, such accommodations already happen on an individual basis.
“We routinely write letters for patients to request ergonomic adjustments, movement breaks or flexibility at work or school,” he said. “ADHD has a clear neurobiological basis, and movement helps regulate attention.”
He added that greater awareness could ease communication challenges. “Schools and institutions often don’t understand this immediately,” he said. “Having clearer recognition of the need for movement could make a real difference for patients.”
Movement as access, not preference
Doctors emphasised that the need to stand or move is not about comfort or preference — but about function. “The brain is constantly receiving signals from the body,” Dr Farhan explained. “Posture changes neurotransmitter activity. When you are upright and moving, dopamine and norepinephrine increase, which supports alertness, motivation and focus.”
For people with ADHD or chronic pain, being forced to sit for long periods can worsen symptoms — mentally and physically. Experts say flexible environments that allow people to stand, walk or change posture may not only improve comfort, but also cognitive performance and wellbeing. As modern life becomes increasingly sedentary, doctors argue that rethinking how — and how long — we sit may be just as important as how we work, learn and travel.