Sitting down is supposed to be a way to relax after a long day on your feet. But for many women, sitting for any length of time is painful. It aggravates pain in the back instead of relieving it.
If this sounds like you, the problem could be one of several common conditions, says Dr. Steven J. Atlas, an associate professor of medicine at Harvard Medical School.
One of these conditions is a problem involving one of the discs that act as pads between the vertebrae in your back. In particular, a disc can become herniated, meaning it develops a bulge that can pinch a nearby spinal nerve, causing pain.
"There have been some studies that measured the amount of pressure on the discs," says Dr. Atlas. "Not surprisingly, the pressure is lowest when you're lying down." But there is more pressure on the discs when you're sitting than when you're standing. "In fact, if I come into the exam room and a patient is standing, rather than sitting, my suspicion that the person has a disc herniation goes up a lot," he says.
Disc problems can cause back pain alone, but when the pain moves into the legs, this may be the nerve pain known as sciatica. Sciatica sometimes occurs when a herniated disc pinches one of your sciatic nerves. These are the longest nerves in your body, running from the lower back into each leg. People with sciatica typically report a burning pain that involves the lower back, the leg, and sometimes the foot.
Although the specific reason for back pain often cannot be identified, muscle spasms are probably the most common cause, says Dr. Atlas. While there isn't proof from medical studies that sitting leads to more spasms, people often report tighter and more painful back muscles with prolonged sitting. A long car ride is a typical example. Sometimes people attribute the pain to the jarring and bouncing around that occurs on the road, but often it's just pressure from sitting that triggers the problem.
There is one common condition in older women that is eased by sitting. This is a type of arthritis of the lower back called spinal stenosis.
"In cases where the arthritis is severe enough to pinch nerves going to the buttocks and legs, people often report that the pain is better when sitting than standing. This is because when you sit, you bend forward a little bit at the lower back, and this may spread out the arthritic bones enough to relieve the pain temporarily," says Dr. Atlas. Pain relief may also occur when you lean forward while using a shopping cart or a walker.
When to see a doctor
In most cases, you should be able to manage back pain by yourself. Modify your activity and slowly work toward regaining function, says Dr. Steven J. Atlas, an associate professor of medicine at Harvard Medical School. However, you should see a doctor if the pain isn't improving after you've modified your activity for a few weeks. (It can take up to four to six weeks to see improvement in sciatica from a herniated disc.) You should see a doctor right away if your pain is extremely severe, if it gets better but comes back, or if it occurs after an injury — such as falling down a flight of stairs, being in a car accident, or slipping on a patch of ice. That's different from back pain that begins during the course of regular movements, says Dr. Atlas. In other words, if your back starts to hurt when you lean over to tie your shoe, that's not an injury.
How to relieve the pain
If you're experiencing back pain when sitting, your impulse may be to lie down and then try to slowly progress back to sitting, says Dr. Atlas. But this is the wrong approach. You should lie down to relieve the pain, but the goal should be not to return to sitting, but rather to regain your ability to stand and move. "The goal isn't to get into the chair. The goal is to start moving. Walking is better than sitting," he says. Movement is often the best medicine when it comes to relieving pain.
Treating back pain
If you can't manage your back pain yourself and opt to see a doctor, it's likely she or he will order treatments that follow a course similar to what you can do at home.
"There has been a shift away from medical intervention for back pain and an increased emphasis on treatments that don't focus on medication," says Dr. Atlas. "There is also an increased appreciation that even medicines such as acetaminophen have risks, particularly in older adults."
A typical course of treatment starts with activity modification, progressing to exercise. "For patients with severe symptoms, the first line of therapy might be manual treatment, such as massage, chiropractic, or physical therapy," says Dr. Atlas.
Preventing problems
Movement is the best way to ward off back pain. Regular physical activity can make the back stronger to reduce future episodes of pain. Exercises should focus on increasing strength and improving range of motion — as well as ensuring balance on both sides of the body, as some back pain can start when one side of the body is stronger than the other.
In addition, whenever possible, avoid prolonged sitting. If you sit at a desk in the office all day, get up periodically — at least every 30 minutes — and walk around. Walk to get a drink of water or to pick up your mail. Take breaks throughout the course of the day to prevent future bouts of pain.
A strong back is a healthy back
Some simple exercises (done with the approval of your doctor) can help keep back pain at bay. These exercises build not only strength, but also flexibility. For more tips and exercises to help your back, check out the Harvard Special Health Report
Back Pain: Finding solutions for your aching back (
www.health.harvard.edu/lbp).

Lie on your back with both knees bent. Pull one knee toward your chest and hold it for 5 to 10 seconds. Return to the starting position. Repeat with the other leg. Do this 5 to 10 times with each leg.

Lie on your back with both knees bent and your feet on the floor. Pull both knees toward your chest and hold for 5 to 10 seconds. Return to the starting position. Do this 5 to 10 times.

Lie on your back with both knees bent and your feet on the floor. Gently flatten your lower back to the floor and hold for 5 to 10 seconds, then relax. Do this 5 to 10 times.

Lie face down on the floor, your bed, or an exercise mat. Bend your torso upward and rest the weight on your forearms. Gently arch your lower back and hold for 10 seconds, then relax. Repeat 5 to 10 times.

Start on your hands and knees. Lift and straighten one leg, extending it gently backward without lifting it above your body level. Hold the position for 5 seconds. Do this 5 to 10 times with each leg.
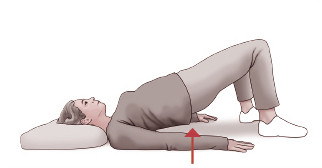
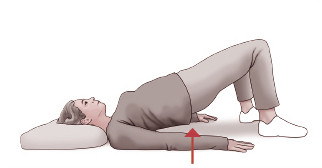
Lie on your back with both knees bent and your feet on the floor. Gently raise your buttocks off the floor 4 to 6 inches, hold for 5 seconds, and return to the starting position. Do this 5 to 10 times.
Image: LaylaBird/Getty Images
https://www.health.harvard.edu/pain/dont-take-back-pain-sitting-down