From gulfnews.com
Modern to alternative medicines, all you need to know about treating sciatica
A searing pain down the back of the leg is usually a sign of sciatica. Life with sciatica is troublesome: simple acts like sitting or picking something off the floor can be excruciating. Here’s an explainer that includes accounts from people who suffered from sciatica, and treatment options: Modern Medicine, Traditional Chinese Medicine, Indian traditional medicine Ayurveda, and Homeopathy.
‘My battles with spinal problems’
A shaft of pain shot through my left leg. It was like a burning sensation down the back of the thigh. Scary, indeed. That was around 15 years ago, my first bout with sciatica.
A trip to an orthopaedic expert followed. The doctor attributed it to prolonged sitting at the desk and poor posture. An Xray followed by a course of anti-inflammatory medicines were only a prelude to physiotherapy sessions. They helped, and the pain went away as I continued to do the exercises prescribed by the physiotherapist.
A few years later, the pain was back. I knew the reason: my unhealthy desk routine and worse, I ignored the exercise. The regimen was repeated and there was relief. And it hasn’t been back. Yoga helped especially surya namaskaram, or the sun salutation.
Now I am back with the same doctor. My lumbar region is fine, but the cervical area is sore and painful. Long hours hunched over the computer followed by some more poring over the cellphone made matters worse.
I ignored it and went swimming and played badminton. A pinched nerve was the result. It was excruciating to lie on my back and two fingers became numb. Disc degeneration is the cause, the doctor said, adding that the space between some vertebrae has been reduced drastically.
Sciatica is no longer a worry, but I’m battling cervicalgia.
— Shyam A Krishna, Senior Associate Editor
‘The excruciating pain radiated down my leg and consumed every aspect of my life’
It all began with a twinge in my lower back, an innocent whisper of discomfort that soon transformed into a spasm — that would come and go. Simple tasks like bending down or sitting for more than a few minutes became challenges. The pain was unrelenting at times as if my body was waging a war against itself.
Yet there were days when I was completely fine. The doctors said I suffered from a compressed disc. It was the pressure from my herniated disc that irritated the sciatic nerve, causing pain.
The excruciating pain radiated down my leg and consumed every aspect of my life. Sometimes I would wake up in the morning with a stiff back. Sciatica had become an unwelcome companion, casting a shadow over my life.
The intensity of the pain ranged from mild to severe, and it worsened with certain activities like sitting, standing, or walking.
However, little did I know that within the depths of despair, I would find the resilience to triumph over this debilitating condition. I refused to let it define me.
An appropriate treatment plan and proper guidance on exercises helped. Physical therapy and exercises to strengthen the core became my sanctuary — a place where pain and hope intertwined.
With each workout session, I pushed myself beyond my perceived limitations. Finally, after what seemed like an eternity, I emerged on the other side. The pain that had once defined me had been reduced to a mere memory.
— Sadiq Shaban, Opinion Editor
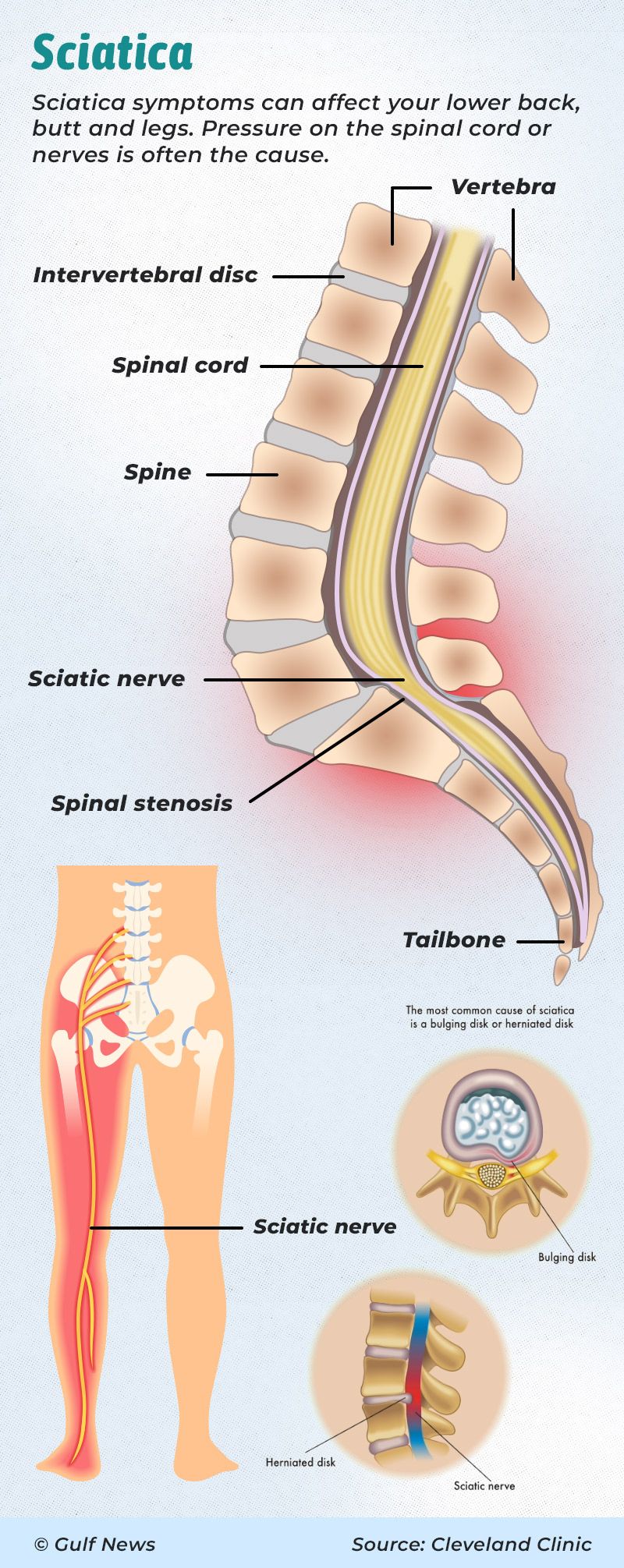
What is sciatica?
Sciatica refers to the pain that originates in the lower back, goes into the buttock and travels down the leg. It can also manifest as weakness, numbness, or tingling in the leg. It is caused by irritation or injury to the sciatic nerve or pressure on it.
How modern medicine diagnoses and treats sciatica
"A Dubai-based taxi driver approached me for sciatica treatment. To diagnose the condition, we asked him to walk on the toe or heel and asked him to rise from a squatting position, which was extremely difficult for the patient," said Dr Amit Kumar Krishna, Specialist Orthopaedics Surgeon, Aster Hospital, Dubai. Lifting the affected leg while lying down will worsen the sciatica pain, said the Dubai-based orthopedic surgeon.
Sciatica treatment
Anti-inflammatories, corticosteroids, lumbosacral belt, strict bed rest, and physiotherapy are the regular treatment methods, but in some cases, steroid injection around the impinged nerve is required, said Dr Amit Kumar. "If the initial treatments fail and symptoms persist or get aggravated even after six weeks, the patient may need surgery."
How effective is the sacroiliac belt in treating sciatica?
The sacroiliac belt is very helpful in the initial three weeks of conservative treatment as it helps in the mobility of the patient and during the patient's daily activities, it also restricts movement like forward bending and an abnormal twist of the spine, which may aggravate the symptoms, said Dr Amit Kumar.
How Chinese medicine treats sciatica
According to Chinese medicine, sciatica is typically seen as an imbalance or blockage of Qi (vital energy) and blood flow in the meridians of the body, said Dr Liu Xin, Traditional Chinese Medicine Practitioner, Wellth, Dubai.
To treat sciatica, Chinese medicine aims to restore the balance of Qi and blood, promote circulation, and alleviate pain, said Dr Liu Xin.
Chinese medicine, which includes various traditional practices such as acupuncture, herbal medicine, cupping Tuina massage, and traditional exercise like taiji, approaches sciatica from a holistic perspective.
The first choice of treatment is acupuncture
Acupuncture points are believed to be located along meridians and can help regulate the flow of Qi and blood; by stimulating these points, acupuncture aims to relieve pain, reduce inflammation, and restore the balance of energy in the body, explained Dr Liu Xin.
“The frequency of acupuncture sessions can vary depending on your specific health condition and the recommendations of your acupuncturist. In general, it is common for individuals to start with more frequent sessions and then gradually decrease the frequency as their condition improves. Typically, weekly 2 or 3 sessions are recommended initially, and then the frequency may be reduced to weekly or biweekly or monthly visits as the desired results are achieved,” Dr Liu Xin said.
This is how Ayurveda treats sciatica
Sciatica, one of the most excruciating and irritating nerve pain, is a common health problem encountered by Ayurveda practitioners, said Dr V L Shyam, Medical Director, Shyam’s Ayurveda Centre, UAE.
Ayurveda comes with the experience of treating Sciatica for over 2,500 years. The condition was identified and recorded in 700 BC by Sushrutha (father of Surgery as per Ayurveda texts) and he named it Gridhrasi. The word Gridhrasi itself suggests that the gait of the patient is similar to a Gridhra (vulture) — whose body is bent towards one side while walking, and abnormal throwing action is seen in the affected leg. Another meaning of Gridhrasi is the deep piercing and pulling pain as if a ‘vulture eating flesh with its beak’, explained Dr Shyam, quoting ancient Ayurveda texts.
Ayurveda elaborates on two types of sciatica: Vata-dominated and Vata-Kapha dominated. The classical signs and symptoms of Gridhrasi mentioned by Ayurveda are pain, intermittent pricking sensation, stiffness and rigidity; twitching or pulsating pain, numbness and sensory loss felt in areas: low back, waist, buttocks, thigh, knee, calf and foot, the alternative medicine doctor said.
In the Vata-Kapha type of sciatica, loss of taste, reduced strength in the affected leg and heaviness of legs are seen. The treatment is slightly different in each type, he explained.
What are the recommendations of Ayurveda to tackle sciatica?
Ayurveda book Ashtanga Hrudaya (written in 700AD) mentions that the lifting of the leg is restricted in Gridhrasi. Restricted “straight leg raising (SLR)” is considered as the clinical confirmation of sciatica, he added.
Ayurveda recommends reducing dry foods, lentils and dals, cold food, spicy-bitter-astringent foods, untimely eating, dieting and fasting, overexertion, keeping awake at night, suppression of urges, uncomfortable posture while sleeping, and reducing emotions like stress, grief, fear and anger, Dr Shyam said.
Ayurveda recommends natural medicines to reduce sciatic nerve inflammation and nerve tonics and also advocates a few heat therapies and oil treatments for the relief of sciatic pains. Administration of medicines through the anal tract (Vasthy) and thermo-cautery (superficial burns with heated metallic equipment) are other extensive treatment methods mentioned by Ayurveda for sciatica, Dr Shyam said.
Sciatica prevention: Tips from a Dubai-based orthopaedic specialist

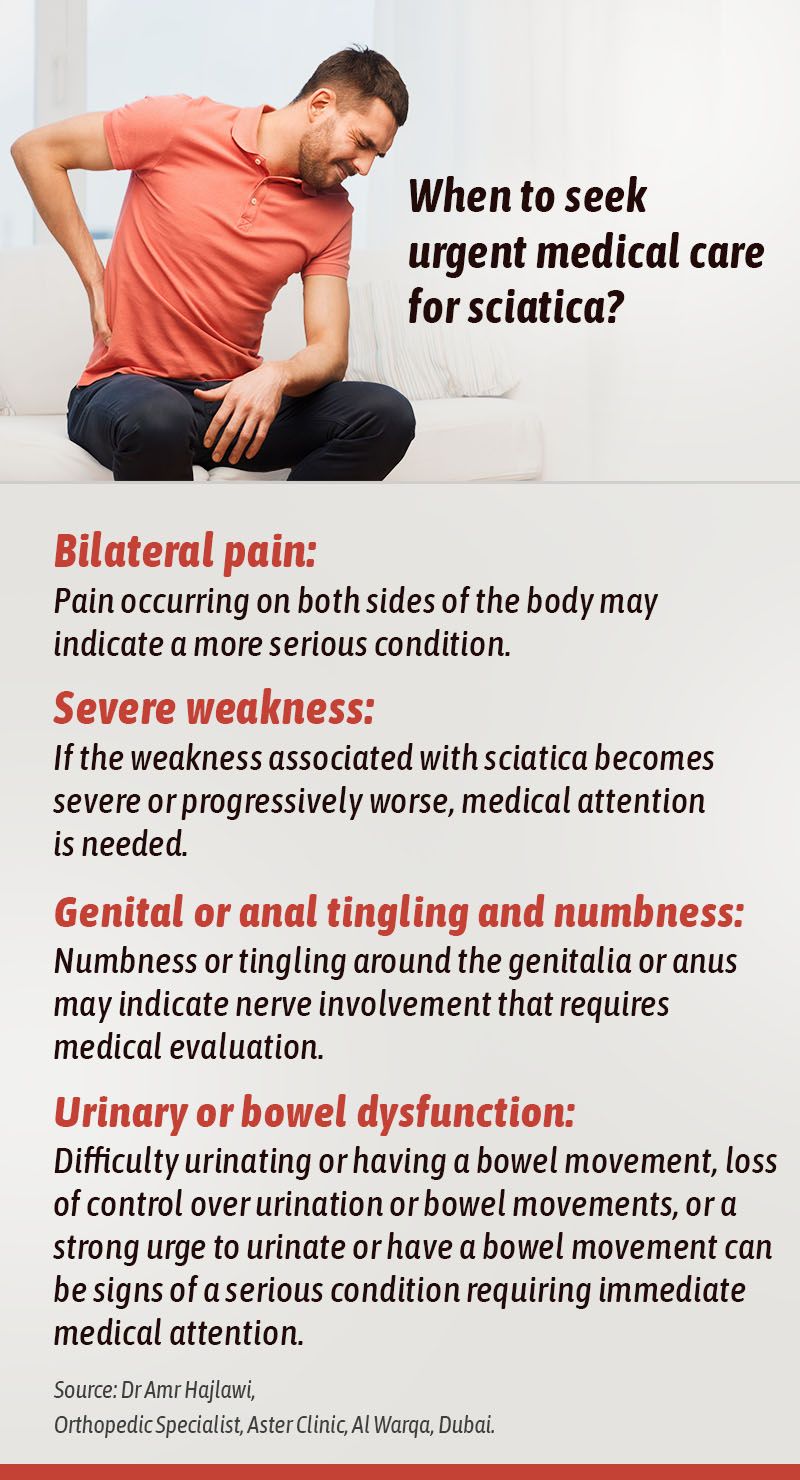
When to seek urgent medical care for sciatica
How to manage and live with sciatica

How Homeopathy treats sciatica
Homeopathy is a system of medicine that treats patients on symptom similarity. To treat the patient: symptom presentations, disease history, family history and when and how often the pain worsens are all taken into consideration, said Dr Rosamma Sabu, Balsam Homeopathic Centre, Sharjah. After all of these are considered, a specific remedy will be selected for the patient, she said.
Homeopathy gives importance to patients' tastes
"I remember a patient with left leg pain that increased while lying down at night and was better by walking. The pain was so severe that he couldn’t sleep at night and must walk up and down frequently. He was also diabetic, and whenever he woke up at night, he used to drink cold milk. He could not explain the reason, but it was one of his favourite drinks," said the Sharjah-based Homeopath.
Homeopathy gives importance to the tastes of the patient, and taking all aspects into consideration a treatment plan was selected and given for 15 days, Dr Rosamma said.
The patient returned on the 15th day complaining that the pain remained the same, but his sleep quality was much better. The same medicine was repeated for a month, and he came back after six months and said that the pain reappeared in winter. The medications were continued for another month and he never had the same problem again, the Homeopath said.
Here is all you need to know about sciatica
What’s the sciatic nerve?
The sciatic nerve is the largest single nerve in the human body. Formed of five nerve roots in the lumbar and sacral spine, the sciatic nerve starts in the lower back and runs down the back of each leg.
The body has two sciatic nerves, one on each side — the right and left legs. The nerve controls the muscles on the back of the knee and lower leg. It also provides sensation to the back of the thigh, the outer and back part of the lower leg, and the sole, according to a report on the US-based Cleveland Clinic’s website.
What are the types of sciatica?
There are two types of sciatica: true sciatica and sciatica-like conditions. True sciatica is the pressure or injury that directly affects your sciatic nerve. Sciatica-like conditions feel like sciatica, but it does not result from an injury or pressure to the sciatic nerve. Other reasons could be linked to the sciatic nerve or its five roots.
What are the symptoms of sciatica?
The symptoms of sciatica vary widely. Generally, it may feel like a dull ache or burning sensation in the back, running down the buttock to the back of the thigh and the calf. It can also feel like an electric shock. Some people experience mild tingling, weakness or numbness in the leg or hip.
The symptoms can be infrequent in some cases, while there are cases when they can be so severe and debilitating that a person cannot move. It mostly occurs on only one side of the body.
The pain starts slowly and may worsen after standing or sitting. If sciatica stems from a compressed disc, patients will feel pain while sneezing, coughing or laughing. In other cases, pain occurs while bending backwards or walking. It may happen when straining or holding your breath.
How is sciatica diagnosed?
Healthcare providers use a combination of methods to diagnose sciatica. Generally, the symptoms give a fair idea. A report in Penn Medicine of the University of Pennsylvania says, besides flexibility and strength checks, they will also conduct a physical examination to find out the following:
- Visible changes in walking
- Weakness when bending the knee
- Difficulty bending the foot inwards or down
- Difficulty walking on toes
- Difficulty bending forward or backward
- Abnormal or weak reflexes
- Loss of sensation or numbness
- Pain when lifting the leg straight up while lying on the back
What are the tests to diagnose sciatica?
Several tests can help in diagnosing sciatica and ruling out similar conditions. The most common tests include:
- X-rays or computed tomography (CT) scans
- Magnetic resonance imaging (MRI) scans tests of the spine
- Nerve conduction velocity studies
- Electromyography: It measures muscle response to a nerve’s stimulation
- Myelogram: A diagnostic imaging test used to look for problems in the spinal canal
How common is sciatica?
Sciatica is a very common condition. About 40 per cent of people experience some form of sciatica, according to the Harvard Medical School. Although it rarely happens before age 20, it becomes more frequent as people age. Men between 30 and 50 are more likely to have sciatica.
About 85 per cent of the population will suffer from back pain at some point in their life, but only between two and 10 per cent will have true sciatica, Canadian chiropractor James Lemieux said on the University of Alberta website.
“People who suffer from acute or chronic back pain tend to be more susceptible to sciatica,” Jeffrey N. Katz, professor of medicine and orthopaedic surgery at Harvard Medical School, said. “Your risk also rises if you’re obese, if you smoke, or if you’re sedentary.”
What causes sciatica?
Sciatica occurs when there is pressure on the sciatic nerve. It could also result in an injury. The common causes are:
Slipped or herniated disc: When the soft tissue between the bones (vertebrae) in your spine seeps out
Spinal stenosis: Narrowing of the part of your spine where nerves pass through
Spondylolisthesis: When one of the vertebrae (bones in your spine) slips out of position
Back or pelvic injury
Piriformis syndrome: A pain disorder involving the narrow muscle in the buttocks
Tumours, cysts or other growths
Osteoarthritis
Pregnancy
What are the major risk factors for sciatica?
Some of the many potential risk factors listed by the Cleveland Clinic include:
Injury: Injuries to the spine or lower back increase the risk of developing sciatica.
Wear-and-tear: As people grow old, normal wear-and-tear on the spine can lead to pinched nerves, herniated discs and other conditions that can cause sciatica.
Obesity: A big belly or paunch can weaken the muscles in the back, leading to back strains, pain and other issues.
Insufficient core strength: The strength of the “core” (muscles of your back and abdomen) is vital as abdominal muscles anchor the back muscles.
Jobs: Works that involve heavy lifting, a lot of bending, or working in awkward or unusual positions may increase the risk of back problems. Prolonged sitting without proper back support may also increase your risk.
Posture: Good posture and proper form are important when lifting heavy objects, weight lifting, strength training or similar activities. Or else it can lead to back problems.
Diabetes: Type 2 diabetes increases your risk of peripheral neuropathy. That damages your nerves, including any of the sciatica nerves causing or contributing to sciatica.
Physical inactivity: Prolonged sitting and a lack of physical activity can increase the risk of sciatica.
Tobacco: Nicotine use can affect circulation and raise the risk of chronic pain, including sciatica.
What are the complications of sciatica?
Most people recover from sciatica within four weeks of treatment. In some cases, it may extend to a year.
A possible complication of sciatica is chronic or long-term pain, which results from unrelieved nerve compression. The main complications, according to the Health Encyclopaedia of the University of Rochester Merical Centre in the US, are:
1. Increased pain
2. A slipped or herniated disc
3. Loss of feeling or weakness in your affected leg
4. Loss of bowel or bladder function: Surgery will be necessary.
5. Permanent nerve damage: It could lead to chronic muscle weakness, such as a “drop foot,” making walking difficult or even impossible.
How is sciatica treated?
No treatment is required in mild cases, and recovery occurs over time. Bed rest is NOT recommended. Start mild exercises after the pain dissipates. But continued pain will require treatment, depending on the severity of the condition.
Self-treatment
In cases of mild pain, self-treatment can be helpful. If the pain doesn’t go away, seek professional help. These are some self-help tips from the Harvard Medical School:
1. Reduce physical activity for the first few days before resuming them slowly.
2. Avoid lifting heavy objects, and do not twist the back.
3. Ice or heat packs: They can help reduce pain and swelling during the first few days of pain. Apply ice packs (wrapped in a towel) for 20 minutes at a time, several times a day. After the first several days, switch to a heating pad or warm compress. Apply heat for 20 minutes at a time.
4. Physical activity: This is best learnt from a physiotherapist or a sports medicine expert. It will strengthen core muscles.
5. Seek professional help: If the self-care doesn’t help after a few weeks, it’s time to consult a doctor.
Regular treatments
Prescription medications: Painkillers, muscle relaxants and other medications may help relieve sciatica symptoms.
Physiotherapy: A physiotherapist will ask the patient to do exercises to reduce pressure on the sciatic nerve. Stretching exercises, walking, swimming and water aerobics will also help.
Spinal injections: Injections like corticosteroids may provide short-term relief (typically up to three months). But this is no substitute for therapies that give long-term relief.
Alternative therapies: A chiropractor to adjust the spine, yoga, acupuncture and massage therapy might also help.
Surgery
Surgery to relieve the compression of spinal nerves is an option when sciatica is very severe. It is usually a last resort when all other treatments fail.
Doctors recommend surgery only if the pain that prevents a person from carrying out their normal routine. Particularly if the patient has symptoms of nerve damage or a possibility of nerve injury. A Mayo Clinic report said people with severe leg weakness or bowel or bladder changes might need surgery.
Surgery options, according to Johns Hopkins Medicine, include:
Discectomy: It is to remove fragments or small sections of a herniated disk that are pressing on a nerve.
Laminectomy: Behind each vertebra is a section called the lamina. A laminectomy removes a section of the lamina that’s pressing the spinal nerves.
Is sciatica preventable?
Some causes of sciatica can be prevented, but it can also happen for unknown reasons, according to a Cleveland Clinic report. Anything that reduces the risk of nerve damage can only be good. That includes avoiding sitting for long hours or doing anything that puts pressure on the buttocks.
Here are some tips from the Cleveland Clinic to reduce the risk of sciatica:
Good posture: Maintain a good posture while sitting, standing and sleeping. Use a good technique (bend the knees) while lifting heavy objects to reduce stress on the back.
Avoid tobacco: Nicotine from smoking or vaping reduces the blood supply to your bones, weakening the spine and its components.
Body weight: Maintain a healthy weight by eating nutritious food. Calcium and vitamin D are good for bone health.
Physical activity: That should include stretching and strength training. Increasing core strength and flexibility is good for back pain. Aerobic exercises can also help maintain a healthy weight.
Managing sciatica is all about pursuing a healthy lifestyle. Physical activity and strengthening core muscles are key to a pain-free life. So, get moving.

No comments:
Post a Comment